Medication Adherence: How Employers Can Help Employees Be Healthier
The old saying goes: “the most expensive medication is the one you didn’t take.” If that rings true, why is skipping medications so common?
The stats are staggering. Today, nearly 50 percent of adults ages 20-59 take prescription medications, and half of those are considered non-adherent. Twenty to 30 percent of medication prescriptions are never filled, and approximately 50 percent of medications for chronic disease are not taken as prescribed, according to a review in
As healthcare costs continue to rise, employers are looking for ways to help their people get, and stay, healthy. Addressing medication non-adherence is a great place to start.
Why don’t people take their prescribed medication?
Research shows there are many reasons people don’t take their prescribed medications. One of the top deterrents? Cost. High medication costs can create a financial burden, even when meds have been on the market for years. For example, the four-decade-old EpiPen has seen a 500 percent price hike since 2007.
On top of cost, adverse side effects keep people from taking what the doctor ordered. Twenty-nine percent of patients said side effects prompted them to stop taking a medication, according to
Non-adherent behavior costs the healthcare system $300 billion a year. When patients refuse to take a medication, the risk of hospitalization and lingering health issues can increase. For employers, this means lost productivity and an unhealthy workforce – both creating a substantial cost issue. Of the $300 billion, $100 billion can be attributed to hospitalization and rehospitalization that could have been avoided if medications were taken as prescribed.
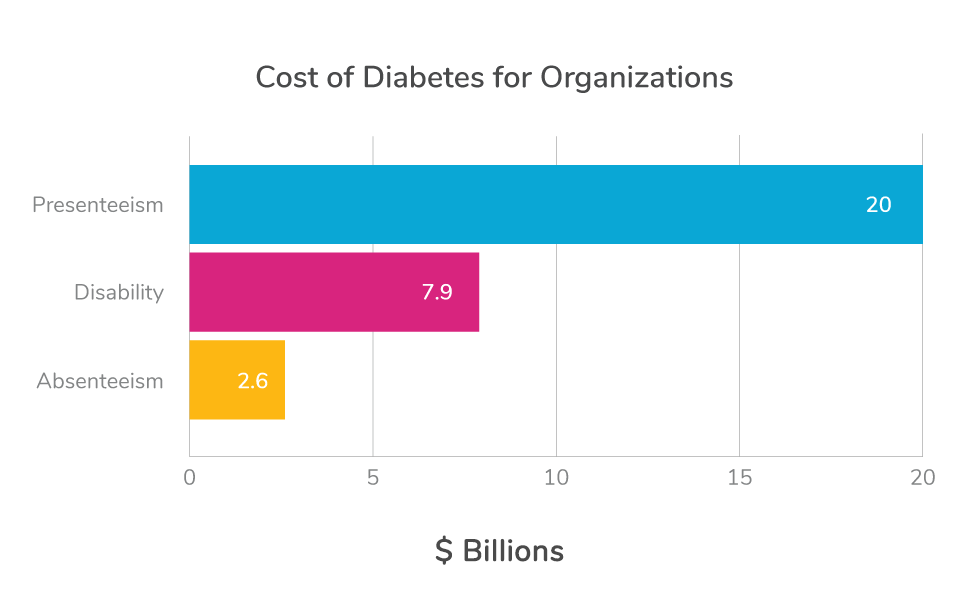
Employers bear the financial burden of lost productivity when employees are hospitalized due to avoidable health incidences. Take diabetes, a leading chronic condition impacting nearly 30 million Americans, for example. Annual diabetes-related direct medical spending is likely to grow to $336 billion by 2034. Employers take on a major part of this direct medical cost burden and face a significant indirect cost burden. Estimates show diabetes costs organizations $2.6 billion in absenteeism, $20 billion in presenteeism (120 million workdays with reduced performance) and nearly $7.9 billion in annual disability costs.
How employers can impact medication non-adherence
For many employers, the costs associated with medication non-adherence are too high to ignore. But how can an organization encourage people to take their medications correctly without violating their privacy, especially when the reasons they don’t
The truth is employers can impact medication compliance, and they’re in the perfect position to do so. The first step is to examine claims data to understand the problem. Which conditions have the highest claim data? Is there is a significant number of complications or readmissions that are associated with not taking medication?
Armed with this information, employers can shape the benefits and programs they offer to remove barriers for their employees – whether cost, convenience, side effects, or lack of knowledge – and help them take their medications the way they should.

Taking it one step further – Meet your new pharmacist
A
Think about your last visit to a retail pharmacy to pick up a prescription. It looks something like this: Waiting in line, giving your name and birthdate, taking your prescription and heading out the door. When the pharmacist asks if you have any questions, you will probably say “No.” Maybe you don’t have questions, or maybe you don’t know what you should ask.
The interaction is impersonal. You don’t know your pharmacist by name. Or perhaps, you didn’t even visit the pharmacy, but instead received your medication via mail for convenience. But a mail order doesn’t come with a pharmacist to walk you through how to properly take it.
This story looks very different when people have access to a dedicated pharmacist through their employer or another organization. Instead of being an impersonal interaction, they have one convenient pharmacy – either onsite at their work or near where they live – and a pharmacist who knows them. It makes it much easier and more convenient to pick up medications, ask questions, and solve problems like side effects and high costs.
How Premise Health increases medication adherence
Through our experience with onsite and
For example, maybe the reason someone doesn’t take her medication is because of prescription prices. Because our pharmacists serve one organization, they know members’ benefits plans inside-and-out. They can help members identify less expensive options, or work through issues with insurance. Or, if a member isn’t taking his medication because it has side effects, our pharmacists can offer guidance on how to avoid them – or work with the member’s provider to find an alternative.
Through our onsite and nearsite pharmacy model, we:
- Facilitate communication among the provider team: Our pharmacists work closely with members’ providers. They can alert them when a member isn’t taking his or her medication, which helps the physician better serve that member. It’s a team-based approach that can lead to better outcomes.
- Tap into the power of electronic health records: Our onsite and nearsite health centers all use the same electronic health record. That means pharmacists can see members’ history and understand more about their conditions. They can see whether or not members are filling their medication, which allows them to reach out proactively if it looks like a member is non-adherent.
- Train pharmacists differently: Pharmacists graduate with deep knowledge of medications and their uses and complications. We offer additional training and certifications to help our pharmacists identify members who are non-adherent or at risk for complications and proactively engage them.
- Understand members’ benefits: Our pharmacists are dedicated to one or a handful of organizations, and they know the organization’s benefits plan inside and out. They are a powerful resource for members, with the ability to assist with authorizations and make recommendations for alternative medications if something isn’t covered.
Your interaction with the onsite or nearsite pharmacist looks a little different with this approach.
You visit your onsite pharmacist to pick up a prescription. There is no line. The pharmacist greets you by name and asks about your recent vacation. They know you. Then, the pharmacist walks you through how to properly take the medication and potential side effects. They reassure you that if there are adverse side effects, they will be there to talk through alternatives. They walk you through costs, knowing what is and what is not covered by your organization’s health plan. The pharmacist then spends 10 minutes answering your questions to ensure you’re confident, before sending you on your way.
It’s a proactive approach that is proven to drive behavior change, leading to a healthier, more productive population.
- See the onsite pharmacy in action: For a large manufacturer in South Carolina, our onsite pharmacy benefit resulted in an 87% medication adherence rate and a reduction of approximately $1,050 in healthcare expenses per enrolled member per year.
- Learn more about our approach
to onsite
Next on industry insights.

How to Futureproof Your Healthcare Benefits
Read the Blog
Why Partnering with an AAAHC Accredited Organization is a Win for Your Workforce
Read the Blog