From Insights to Impact: Addressing Behavioral Health Gaps Proactively
Imagine giving your care teams the ability to see the full picture of a member’s behavioral health journey — from past diagnoses and missed prescriptions, to ER visits and everything in between. By leveraging claims data, you can uncover deeper insights that empower you to make strategic decisions about how care is delivered to your employees with behavioral health concerns. These kinds of insights can be the difference between a last-minute counseling appointment and an inpatient hospitalization.
But first, what are population health insights?
“Data” is more than a buzzword — it’s a strategic business imperative and public health interest. Population health insights refers to the information that can be found in your medical and pharmacy claims data and your enrollment data, including member demographics, healthcare utilization, risk scores, preventive care, chronic disease prevalence, and pharmacy costs. This data can reveal trends among your employee population, offering a unique lens into how you can improve healthcare outcomes. When combining population health insights with a focus on behavioral health, it can provide transformative benefits.
Here are four key benefits of incorporating population health insights into your behavioral healthcare strategy.
1. Optimized Behavioral Healthcare: The Right Care at the Right Time
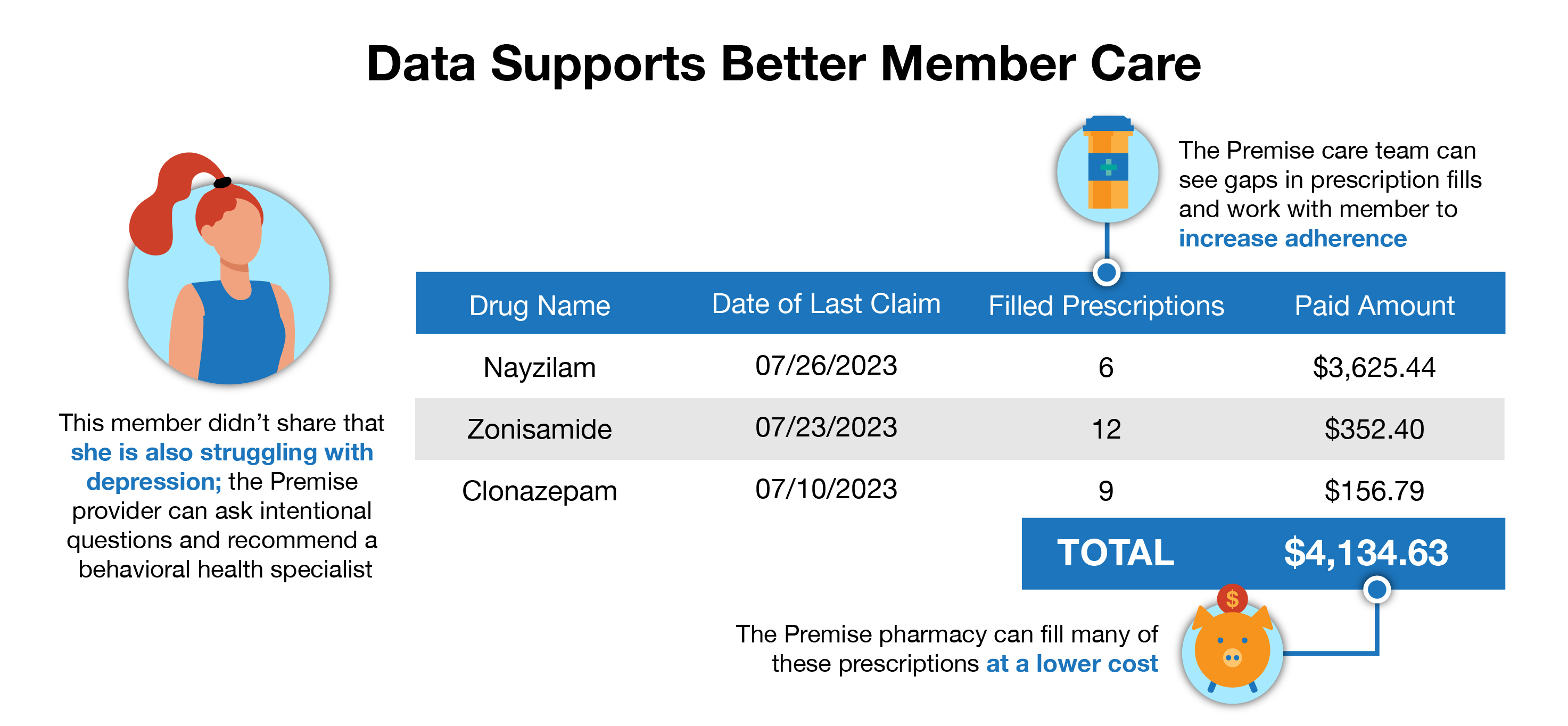
Behavioral health challenges are complex, often requiring tailored, and timely, interventions. A typical office visit with a provider is often not enough time for a member to share their full health history and relevant details, especially when it comes to behavioral health concerns. One of the greatest advantages of population health insights is the ability to empower care teams with data, at the right time. By analyzing claims data and integrating it into member outreach efforts, healthcare providers are proactively equipped with comprehensive information on an individual’s health journey, allowing them to provide support for a member before it’s an emergency.
For instance, by looking at the data and identifying gaps in care — like unfilled prescriptions for mental health medications or lack of follow-up on previous diagnoses — Premise providers can address these issues head-on. They can offer personalized guidance to the member at their next appointment and make necessary referrals to behavioral health specialists, if necessary.
2. Strategic Insights: Aligning Care with Business Goals
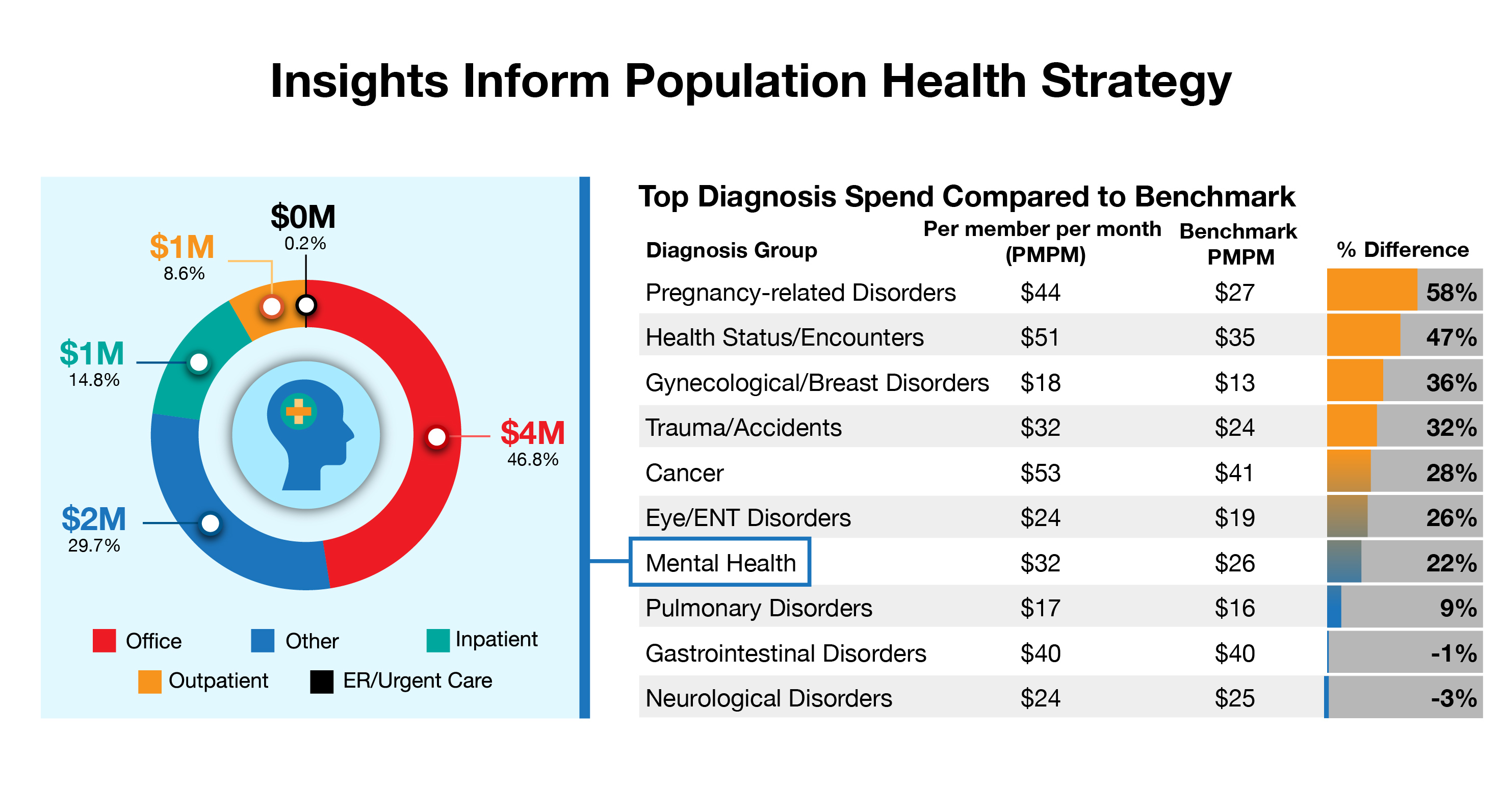
Going beyond individual care, population health insights enable you to identify trends and develop long-term strategies that align with your organization’s healthcare goals and benefits. For example, if your data reveals high behavioral health spend in the community, an onsite, nearsite, or virtual behavioral health solution could help meet that need in a more cost-effective manner.
We found this to be true for one employer, whose mental health spend was 22% higher than its peers. This large expense was mainly due to outpatient visits, costing the employer over $4 million per year. This client also spent another $2 million a year on mental health inpatient and outpatient care, some of which could have been avoided through preventive care. To help resolve this challenge, we helped them implement an onsite behavioral health program to make care more accessible — resulting in better care and lower costs.
3. Engaged Members: Reaching those Who Need Care the Most
Sometimes it can be a challenge to get your people to go to the doctor, which can leave behavioral health conditions unnoticed or unmanaged. Those with unmanaged behavioral health diagnoses are more at risk for other chronic health issues and expensive emergency care.
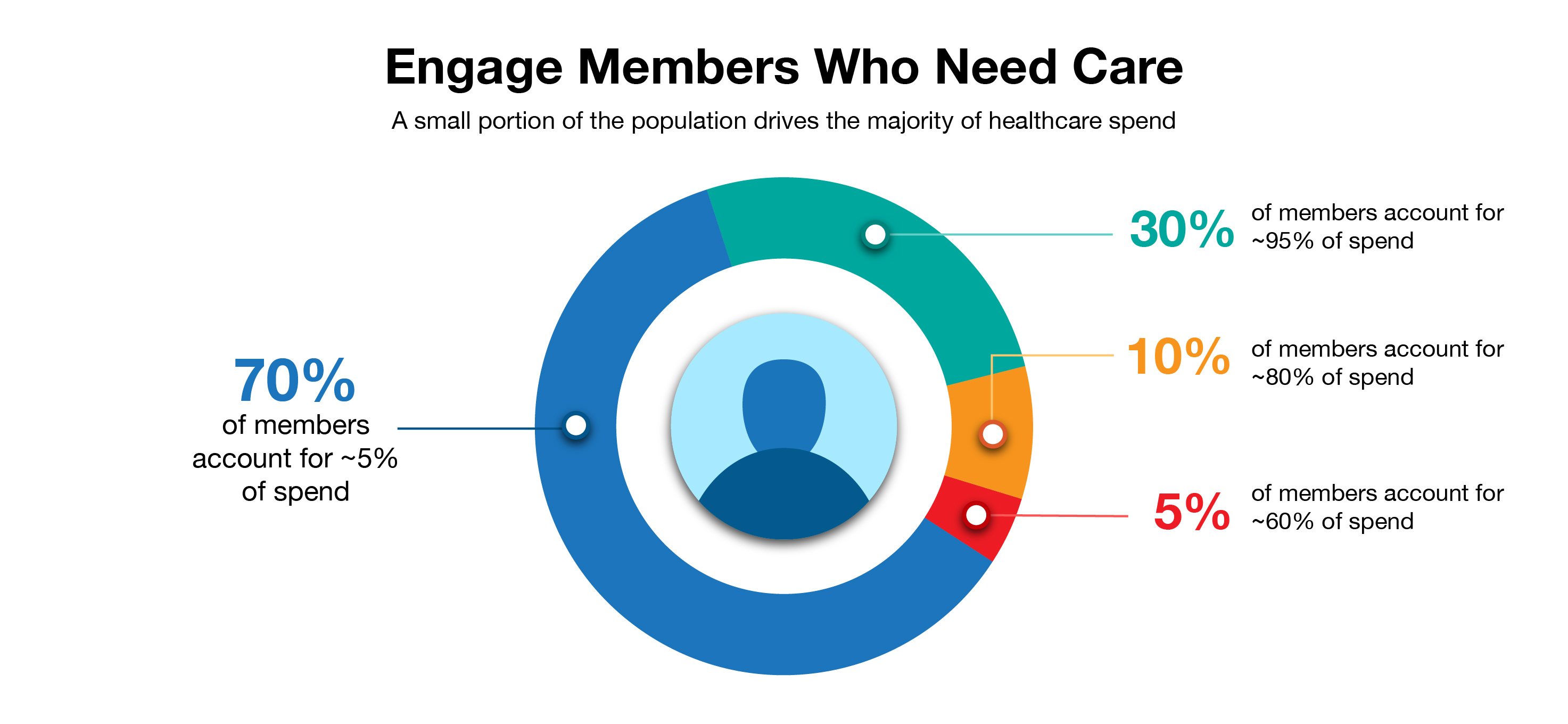
With access to claims data, Premise providers can go beyond traditional population health approaches to proactively identify and work with individuals who are high-cost year after year, as well as those who are high-risk and have unmanaged conditions like depression or anxiety. While it’s important to serve everyone with high-quality care, it’s critical to specifically focus on serving those who need it most.
Take, for example, an employee who frequently visits the emergency room for anxiety attacks. They may not be aware preventive care, such as routine mental health check-ins or medication management, can help prevent these episodes, or that they have helpful resources available through their EAP. By using claims data, care teams can proactively remind the individual about available services and educate them on the benefits of using their onsite, nearsite, or virtual health center for their needs. These interventions not only help improve health outcomes, but also significantly reduce healthcare costs for your organization by addressing issues before they require emergency or inpatient care.
4. Behavioral Health Equity: Breaking Down Barriers to Care
Not all members access healthcare equally. For some employees, managing a behavioral health diagnosis isn’t as simple as making an appointment. Barriers such as past negative experiences, financial concerns, social stigma, cultural differences, or a lack of understanding about available resources can prevent them from seeking care. With a combination of claims data, electronic health records, and survey insights, we can help identify the people who need additional support.
For instance, data may show an individual has missed several scheduled doctor’s appointments. These care gaps can cue their provider to have a conversation with them, either through outreach over the phone or secure messaging via their portal, about their hesitancy to go to the doctor. Let’s say through this conversation, the provider finds out the member hasn’t been taking care of their health because they are worried about costs. Their provider can then direct them to a resource such as Find Help, which offers a list of free community resources and assistance programs for things like food, transportation, and bills. The provider may also make sure the member knows about the low-cost or no-cost health services available to them at their health center, ensuring they feel supported and comfortable seeking care. These efforts not only reduce disparities in access to care but also promote an environment where members feel empowered to take control of their health without fear of financial strain.
From insights to impact, you can take a more proactive approach in improving your population’s mental health. When you can anticipate the needs of your people, you improve health outcomes and reduce downstream care costs. And it all starts with data. See the types of results you can achieve by allowing Premise to manage population health.
Interested to learn more about how population health insights can empower organizations like yours? Contact us today.
Next on industry insights.

Technological Innovation at Premise: A Conversation with Laurel Cipriani, MSc, MSN
Read the Blog
4 Myths Benefits Leaders Believe About AI – and How to Dismantle Them
Read the Blog