Saying Goodbye to Point Solutions: The Movement Toward Integrated Primary Care
Digital health is booming. The COVID-19 pandemic propelled digital healthcare into the spotlight, leading to an influx of new startups, applications, and technologies. Better technology means better data, which should in turn lead to better care and improved outcomes.
However, an unintended consequence of this growth is that employers are overwhelmed by point solutions and a growing benefits tech stack. Many organizations don’t have the bandwidth to ensure each solution is secured, integrated, or optimized.
In response, employers have turned their focus toward benefits solutions that are integrated across the healthcare ecosystem. Employees value having one entry point to all their healthcare benefits, while employers value the increased engagement, utilization and cost savings that comes with it.
The Problem with Point-to-Point Healthcare Solutions
The growth in digital health over the past two years has led to the introduction of numerous new applications and technologies. Many of them are solving gaps in our current care system and provide value to both providers and patients. But taken together, the growth in point solution healthcare benefits is driving fragmentation within healthcare and overwhelming benefits leaders.
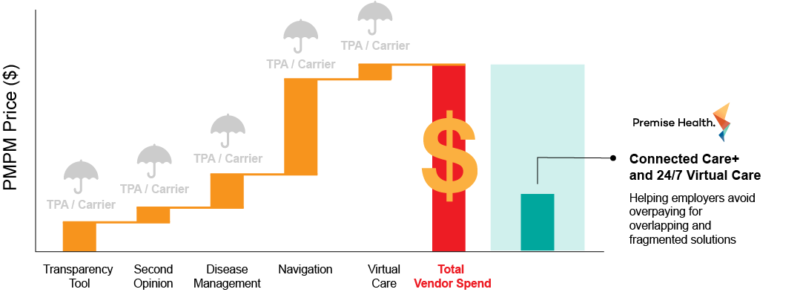
There are many excellent healthcare solutions that do one thing well, such as behavioral health or musculoskeletal care. However, point solutions can have overlapping capabilities, and costs can add up quickly when trying to piece together a comprehensive solution. Additionally, very few of these vendors integrate with one another and the fragmented approach can be overwhelming to patients.
“Healthcare today looks a lot like your iPhone — pages and pages of applications, each serving a single function and operating individually,” shared Jami Doucette, MD, MBA, CSCS, president of Premise Health. “But when it comes to healthcare, each of these applications deals with your confidential patient information, requires constant evaluation by an expert security team, and comes with a high price tag.”
How can organizations avoid some of the challenges of point solutions, while better engaging their populations? It starts with embracing an integrated approach to both your healthcare benefits and primary care.
What Your People Want from Their Benefits
While your employees want the additional benefits provided by new applications, they are unlikely to engage with a service that requires downloading new software, remembering a new password, or interacting with an unknown provider. COVID-19 prompted consumer adoption of new digital modalities, but convenience is still key.
To encourage engagement, your benefits should deliver easy access and a personalized healthcare experience. This typically takes shape as a primary care home that allows patients to establish long-term relationships with a consistent primary care provider team. Today, primary care should encompass not only physical health but also offer holistic care that addresses mental health and social determinants of health. When patients are able to access a trusted physician or provider for all of their healthcare needs, they are much more likely to engage early and often. This means increased utilization, improved outcomes, and decreased costs.
What Benefits Leaders Want from Their Partners
For employers, investing in employee benefits is an important tool for attraction and retention. In order to get credit for the innovative solutions you’re offering, it’s important that your people are aware of all their benefits, have easy access to them, and are encouraged to utilize them. On top of the benefits for your employee population, integrated primary care should mean easy implementation, a trusted partnership, and scalability for your organization.
One of the greatest issues with a growing tech stack is the extra time, effort, and manpower required to implement a new solution or add additional services. When you invest in an integrated primary care solution, you’re also investing in your growth. As you want to add or expand services, you have a trusted partner that can quickly and efficiently adapt your solution. Fewer vendors also means simpler reporting. It’s crucial when investing in a new solution that your team understands how you’ll measure success and has the tools to report on those metrics accurately.
Lastly, what’s good for your employee’s health is what’s good for your bottom line. By delivering a benefits offering that employees actually engage with, your investment should pay dividends, not add additional expenses.
Measuring the Impact of an Integrated Solution
At Premise Health, we know that an integrated approach to care offers measurable cost savings. For example, we studied the cost implications of investing in our comprehensive Connected Care+ and 24/7 virtual care services vs. investing in point solutions for each of the included components. The results were clear. Premise Health delivers the greatest value to organizations and their people by offering one comprehensive approach that ensures members receive high-quality healthcare across the entire ecosystem.
Interesting in learning more? Contact us to see how Premise Health can help your organization today.
Next on industry insights.

Unlocking Better Health: The Power of Advanced Primary Care for Employers
Read the Blog
How Direct Healthcare Can Benefit Unions and Taft-Hartley Funds
Read the Blog