How Social Determinants of Health Impact Wellbeing in Four Graphs
Social determinants of health are the conditions in which people live, work, and play that directly impact health and quality of life outcomes. They include things like access to fresh food, reliable transportation, safe housing, childcare, and more. While these conditions may not come to mind when thinking about a person’s medical health, social determinants of health play a foundational role in overall wellbeing and must be addressed as part of an advanced primary care model.
The following four graphs show the impact several social determinants of health can have on a patient’s health and why these socioeconomic barriers to healthcare are so critical to address.
Food Security
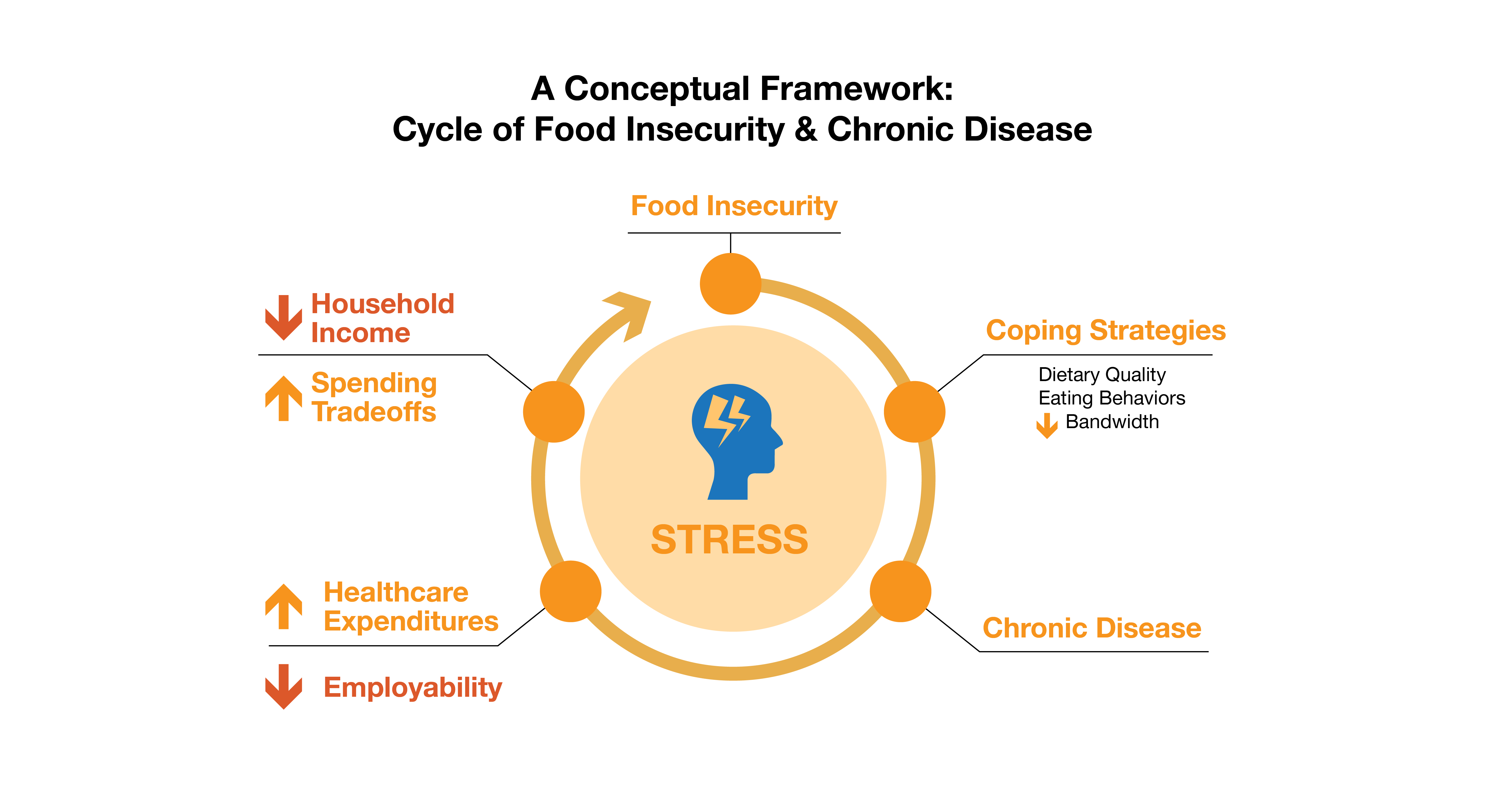
Source: “Importance of Nutrition on Health in America.” Feeding America
Having access to healthy food is an important factor when thinking about someone’s overall health and wellbeing. According to the U.S. Department of Agriculture, food insecurity affects 11% of U.S. households, and this graph shows the dangerous cycle that can happen in those homes. Food insecurity invokes stress, which can in turn negatively impact a person’s health and even exasperate chronic conditions.
For example, one of the factors that determines food insecurity is being under or unemployed. If someone doesn’t have the means to afford everything they need, they will have to make spending tradeoffs. Should money be spent on their important medications? Or should it go toward putting food on the table? Choosing not to purchase medication and stay adherent can make a person sicker, affecting any employment they do have by causing them to miss work. This leads to less income and higher healthcare expenses for follow up visits or specialist appointments, which continues the cycle and makes it harder for a person to find relief.
Transportation
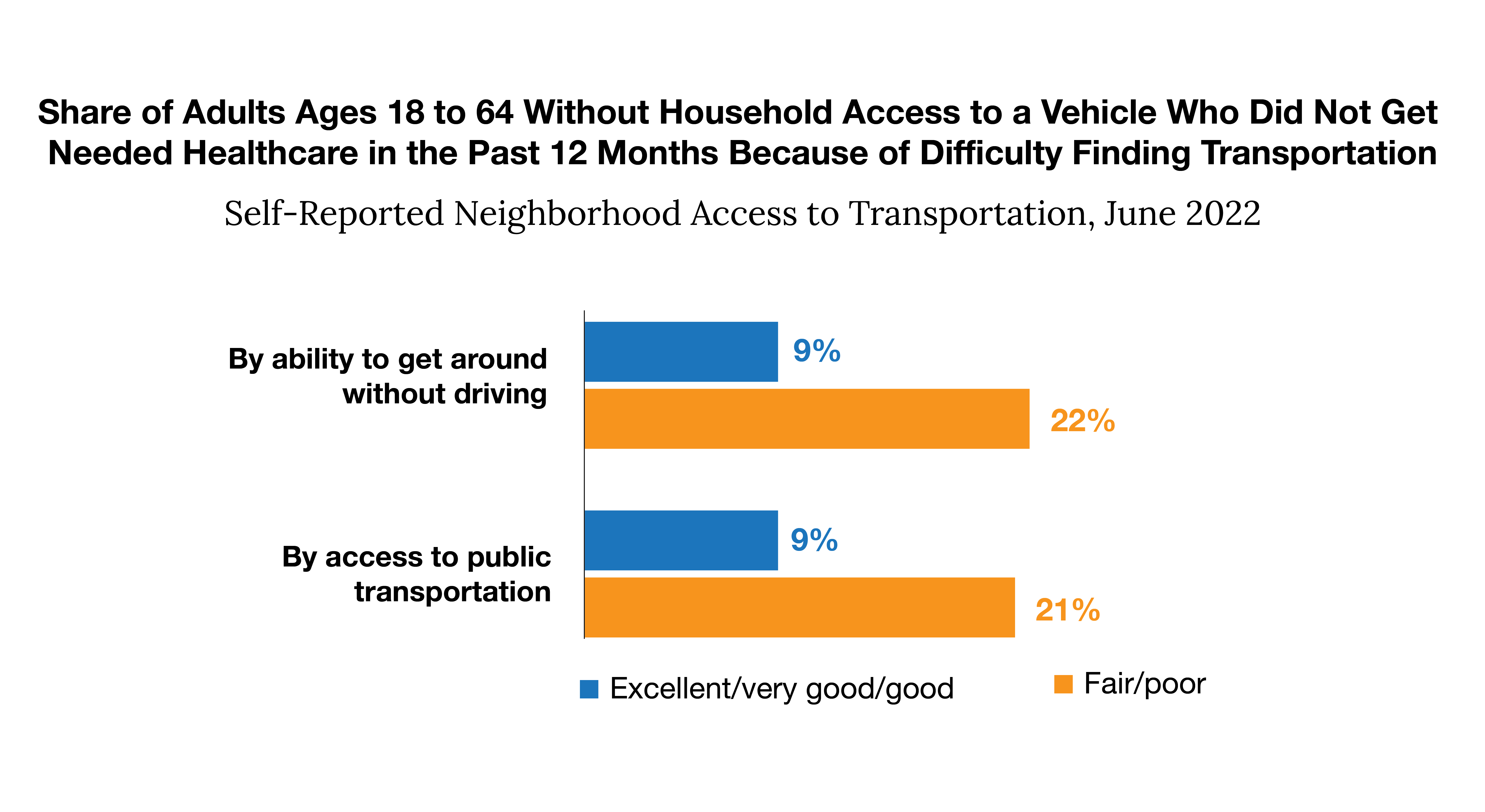
Source: Urban Institute. “More than One in Five Adults with Limited Public Transit Access Forgo Health Care Because of Transportation Barriers.” RWJF, 26 Apr. 2023
Some barriers can make or break a patient’s ability to see their provider. Each year, 3.6 million Americans don’t get the care they need due to transportation issues. This graph drives home that point, showing those without access to a vehicle were unable to get necessary healthcare due to poor access to transportation options. When a person doesn’t own a vehicle, they are dependent on a public transportation system, which are more common in urban cities that rural towns. While it’s great news if there is public transit, the next barrier is financial – does the patient have enough money to afford a bus pass or rideshare?
If someone can overcome their transportation barriers to healthcare, it may be feasible for them to do for once-a-year appointments. However, it may not be within their budget if their medical history requires frequent follow up appointments or separate trips to a specialist or pharmacy. Some offices and health systems tout their virtual care options as a solution for transportation barriers, but it’s not a catch-all solution. Some patients may not have a smart phone, access to internet, or the digital literacy to schedule and complete a virtual appointment.
Physical Activity
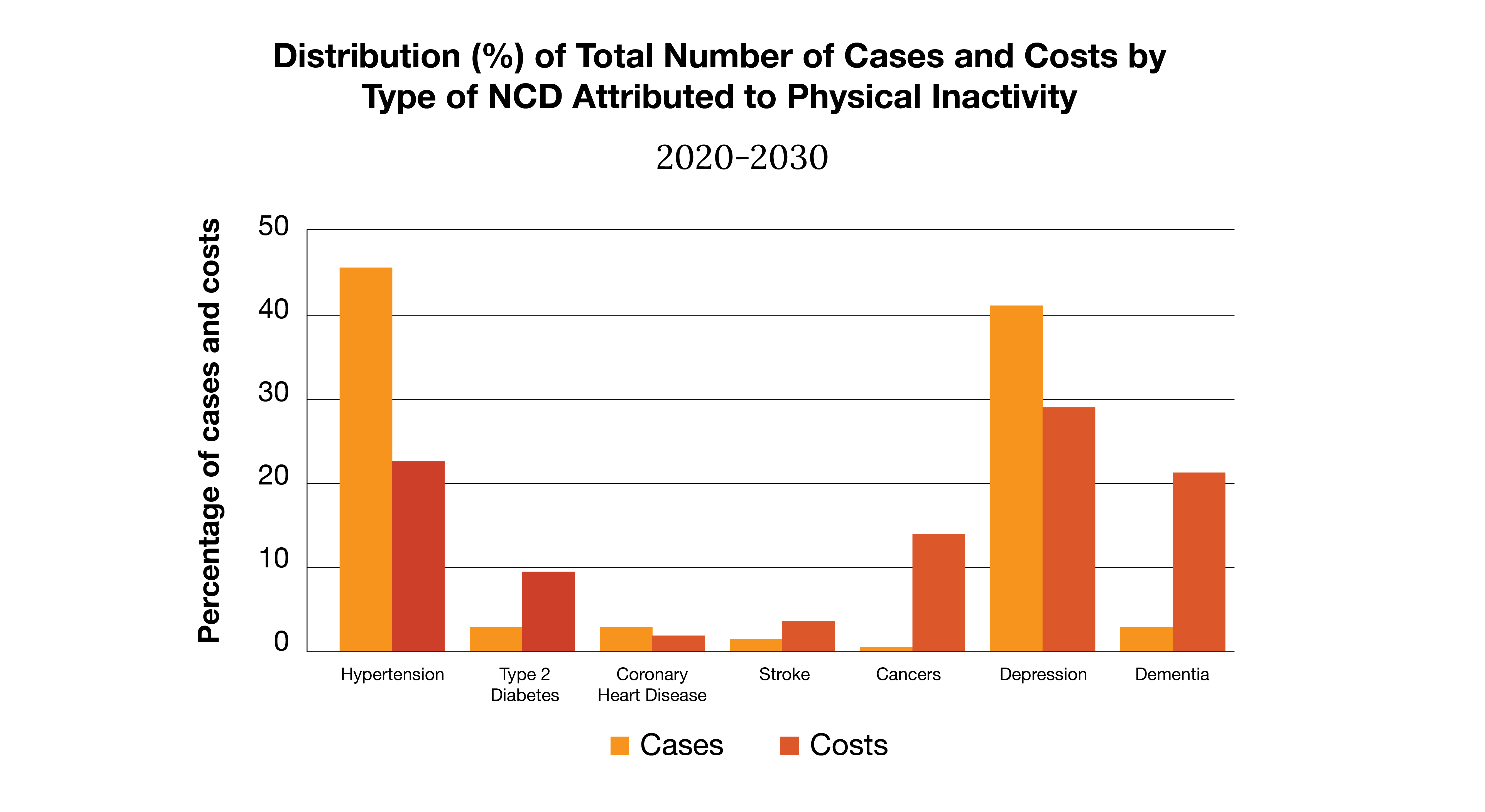
Source: “The Global Status Report on Physical Activity 2022.” World Health Organization, 19 Oct. 2022
We know physical activity can keep us happy and healthy, helping people avoid costly chronic conditions. However, only 28% of Americans are meeting physical activity guidelines set by the Centers for Disease Control and Prevention. A person’s physical environment directly impacts this percentage. If a community isn’t safe to walk around, if there is limited access to parks or safe sidewalks, or if there isn’t a community recreation center nearby, being physically active can be challenging. While many Americans participate in virtual fitness classes or use an at-home gym, not everyone has the means to afford these options. As this graph shows, when physical activity isn’t addressed as a social determinant of health, noncommunicable diseases (NCDs) become more prevalent. This increases costs for both employers and their employees, making it a crucial social determinant of health to address.
Financial Insecurity
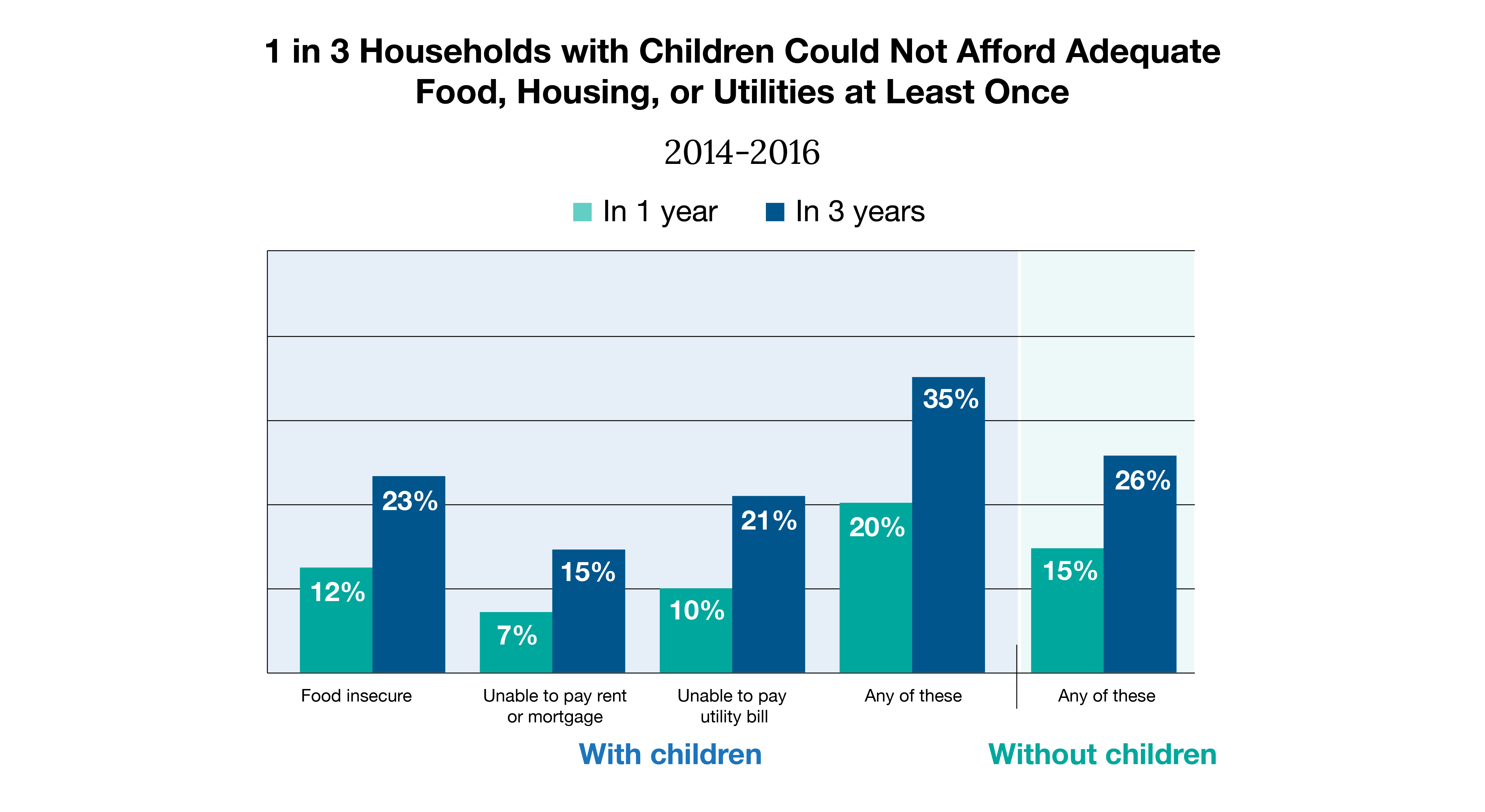
Source: Sherman, Arloc, et al. “Widespread Economic Insecurity Pre-Pandemic Shows Need for Strong Recovery Package.” Center on Budget and Policy Priorities, 14 July 2021
It’s clear that financial barriers are interwoven with many social determinants of health. Nearly 12% of the U.S. population is living in poverty, which forces people to make spending tradeoffs. Choosing to pay for food could mean being short on a mortgage payment, which leaves someone housing insecure. Paying a mortgage but not a utility bill can increase a person’s risk of severe illness. If they don’t have running water to wash their hands with soap and water or electricity to keep certain medications cold, their health will suffer. This graph depicts just how interwoven social determinants of health are and that they often do not stand alone. Many coexist and compound on one another, greatly impacting someone’s quality of life and overall health.
How Premise is Supporting
At our health centers across the country, Premise care teams are asking patients the right questions to ensure we’re providing whole-person care. By asking a series of questions to understand the non-medical factors impacting a member’s health, we can find resources to help get them on a path to better wellbeing. Our electronic medical record has a tool embedded within, Find Help with Premise, which allows providers to make referrals to resources at the point of care. They can help patients find everything from food pantries and shelters to vouchers for free transportation and discounted recreation centers. Our members can also access these resources on their own by visiting www.findhelp.premisehealth.com and entering their ZIP code.
We ask because we care. Reach out to learn more about how we can deliver high-quality, whole person care to your deserving employees.
Next on industry insights.

How to Futureproof Your Healthcare Benefits
Read the Blog
Why Partnering with an AAAHC Accredited Organization is a Win for Your Workforce
Read the Blog