Organizations save $5,377 PMPY when members use behavioral health and primary care
What happens when caring for mental health is just as important as physical health? With 60% of employees identifying work as a key driver of their mental health1, integrating behavioral health with primary care is essential to addressing their needs holistically.
The Findings
This analysis revealed compelling evidence supporting the integration of behavioral health and primary care through an advanced primary care model. Employers and unions realized significant savings for Premise-attributed members compared to those attributed to community providers.
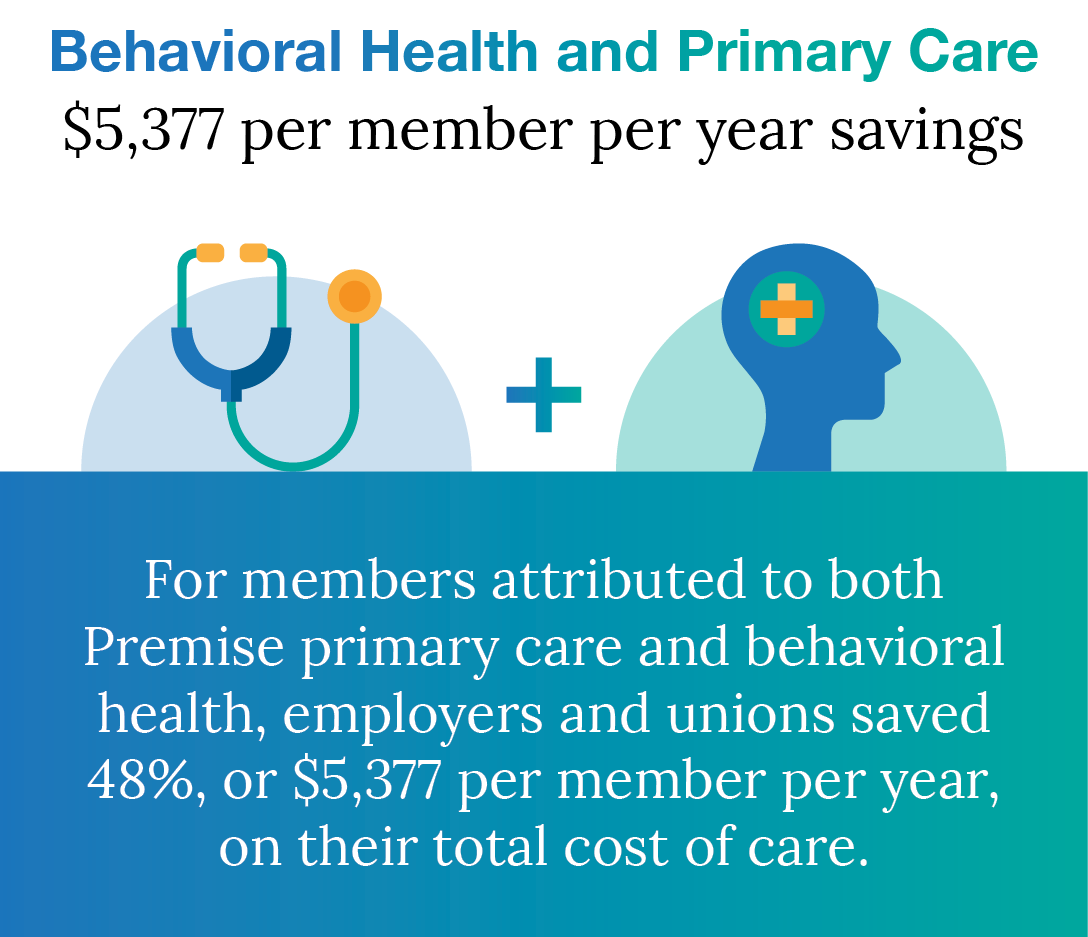
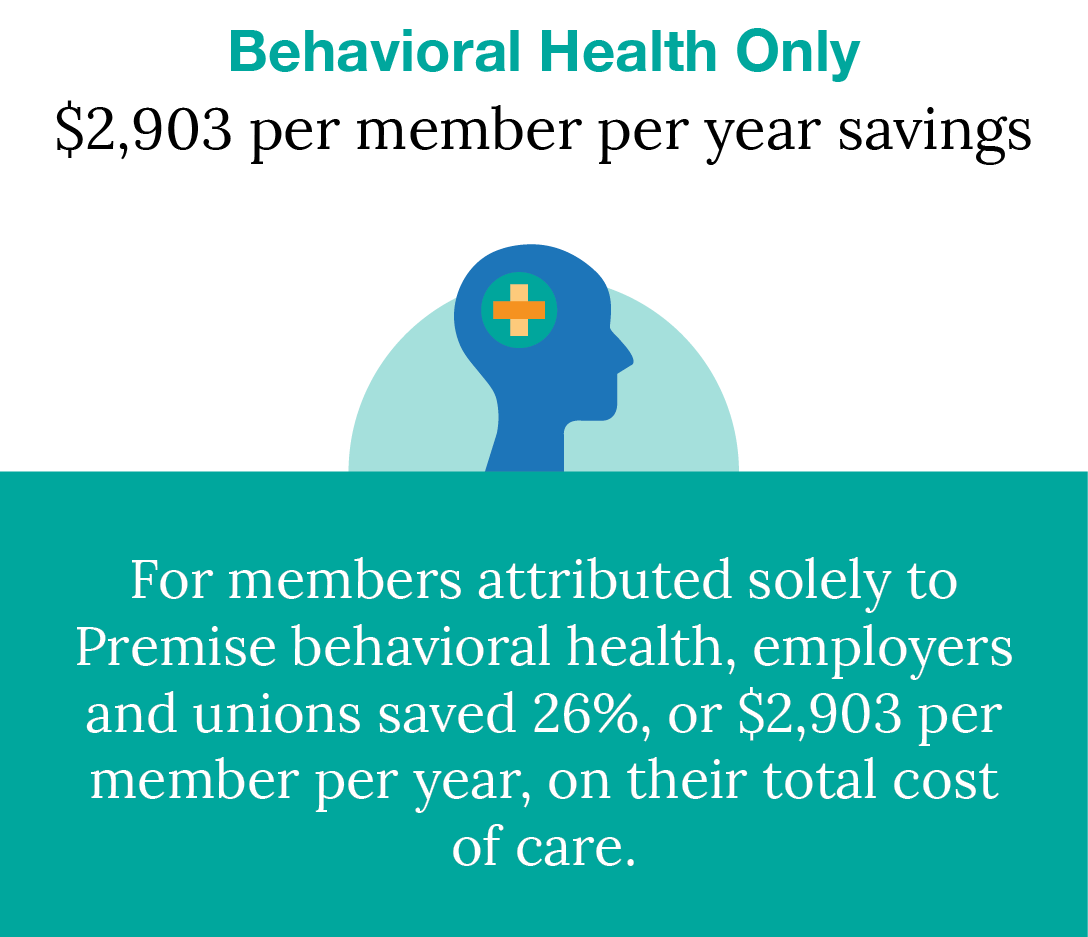
These savings were achieved despite higher age and condition trends among the Premise-attributed population, which typically correlates with increased costs.
More Care = More Engagement
When providers work together on the same care team, their patients benefit by having access to multiple appointment types under one roof. This collaborative, patient-first approach simplifies their experience and makes it easier to get care. Applying this logic to the population studied, the data shows higher engagement as a key result in addition to total cost of care savings.
- 88% of Premise-attributed behavioral health members engaged with primary care services, compared to 68% in the community-attributed group.
- 57% of these members chose Premise as their primary care provider, compared to only 4% of those who received behavioral health services outside of Premise.
Members attributed to Premise for behavioral health pursued 97% of their counseling visits with a Premise provider. This continuity enables more personalized treatment plans, earlier detection of mental health concerns, and reflects the trust and strong connections we build with our members.

Expanding Access to Care
When surveyed, 32% of members indicated they would have received no behavioral health care without Premise. That means countless individuals might have faced a mental health challenge alone or been forced to rely on costly community resources.
More Engagement = Better Health
This increase in engagement led to more preventive care and fewer emergency room visits and hospital admissions. When members have the support of a behavioral health professional, their reliance on other more costly forms of care decreases. The study showed that members who used Premise for behavioral health saw a:
49%
Reduction in urgent care, emergency room, and specialist visits
79%
Reduction in inpatient visits
27%
Reduction in outpatient visits
Integrating behavioral health with primary care is a cornerstone of Premise Health’s advanced primary care approach, which focuses on delivering comprehensive, whole-person care that considers both the mind and body. By caring for mental health with the same importance as physical health members are seen as a person, not just a name on an appointment list, and see better all-around health outcomes.
With healthcare costs and mental health crises both on the rise, offering integrated behavioral health and primary care is one way employers and unions can better serve their people and control healthcare costs.
The Study
Premise Health conducted an analysis of employers and unions within our behavioral health book of business, including over 96,000 unique lives across nine organizations in a variety of industries and geographic regions. It examined how the integration of behavioral health and primary care, a core tenet of Premise’s advanced primary care model, impacts the total cost of care for employers and unions.
Industries represented:
- Automotive
- Finance
- Healthcare
- Insurance
- Labor Unions
- Manufacturing
- Public administration
- Software
The Methodology
This study was conducted using 2023 data and analyzed two distinct groups: members attributed to both primary care and behavioral health at Premise, and those attributed solely to Premise behavioral health. Both groups were compared to their community-attributed counterparts to calculate savings on a per member per year basis, while also accounting for concurrent risks.
For the purposes of this study, Premise attribution was defined as engaged members that have most of their visits with a Premise Health provider rather than with community providers. The community refers to any healthcare provider outside of the Premise ecosystem, including private practices, hospital systems, and more.
“Mental Health at Work: Managers and Money”: UKG. (2023). Mental Health at Work: Managers and Money. The Workforce Institute at UKG https://www.ukg.com/resources/white-paper/mental-health-work-managers-and-money


