How a food production company saved over $1.2M by optimizing specialty care referrals with care navigation
Seeking to help their diverse and multilingual workforce with referrals to high-value, cost effective specialty care, this family-owned poultry supplier partnered with Premise Health to enhance their offering with a primary care-integrated care navigation solution.
The Challenge
Based in northeast Georgia, this organization first began their partnership with Premise in 2004 by offering primary care and pharmacy services to their employees and dependents. Nearly twenty years later their population has expanded to over 7,000 eligible lives, is largely Spanish speaking, and made up of many first-generation Americans.
With many members experiencing the U.S. healthcare system for the first time, their leadership team knew their people would need help navigating in-network providers when referrals were necessary. The fact of the matter is, hospitals provide a wide array of healthcare services; however, they’re not great at everything, and both quality and cost can vary significantly for the same type of care within the same market. The organization required a solution that could direct their people to high-quality, cost-effective care. With an emphasis on providing concierge support to underserved populations, they worked with Premise to improve health equity across their workforce.
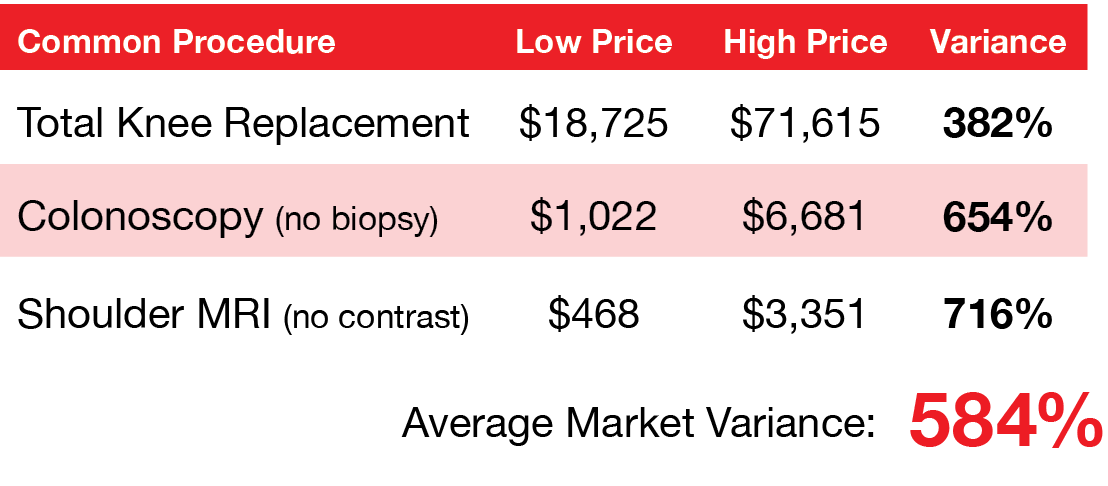
Did you know the price of the same procedure can vary over 500% in the community? To put it in perspective, if gas prices varied as much as procedure costs, you would see anywhere from $2.50 per gallon to $14.60 per gallon depending on the station. On top of that, many stations would be offering a lower quality gasoline for a much higher price.
See what this looks like in one sample market for three common procedures:
The Solution
With the goal of facilitating simplified access to the best specialty care, the organization identified their top priorities:
- Bridge the language gap with an onsite bilingual resource that can help manage referrals
- Reduce total medical spend by optimizing referrals to high-value, cost-effective providers and facilities
- Improve the member experience by enabling people to get to the right specialist and avoid duplicative care
With those goals in mind, the employer expanded their benefits offering to include Premise Health’s referral coordination solution, care navigation. As a core component of an advanced primary care model, care navigation guides members to the highest-value care through data-driven referral matching, concierge support, and integration with a collaborative care team. The onsite wellness center was staffed with a dedicated bilingual care navigator to improve communication with members and ensure referrals for specialty care were sent to the right providers and facilities.
A critical component of advanced primary care.
Care navigation fulfills multiple pillars of advanced primary care, the highest quality of care available:
Enhanced access
Through a concierge approach, care navigators oversee communication and scheduling with specialty providers and facilities to ensure members have access to the right care at the right price.

Team-based
Care navigators keep the members’ care team, including their primary care provider, up to date on follow-up recommendations from specialists.

Outcomes-driven
By focusing on getting members to the right specialist as early as possible, members can avoid unnecessary care and see positive health outcomes sooner.

Continuous
When referrals to specialty care are made, the care team stays connected to the member and closes the loop when they return to Premise as their medical home.
The Outcome
Programs which improve health, reduce spend, and allow providers to engage complex members play an important role in helping employers maximize their healthcare dollars and resources. By expanding their offering to include care navigation, the organization was able to drive optimized referrals, see significant overall savings, and improve member care.
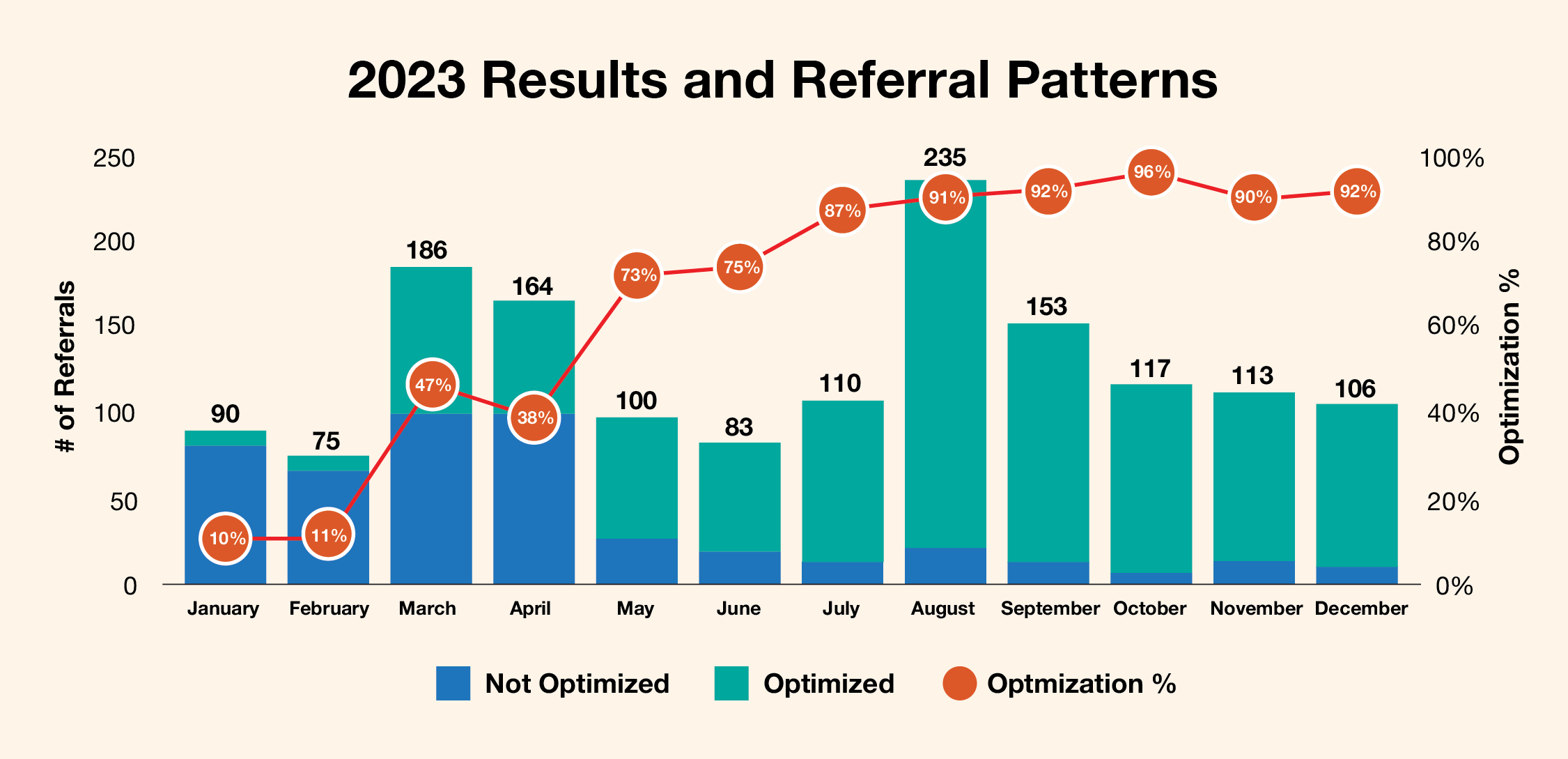
Optimized Referrals
In order to direct members to the best specialists and facilities, Premise care navigators evaluate cost and quality data, direct contracting, payer networks, and EAP programs for every referral. Of 1,532 total referrals from the organization in 2023, 69% or 1,064 were sent to high-value, cost-effective specialists and facilities. As the year continued, the number of optimized referrals began to increase drastically compared to the first quarter, underscoring the effectiveness of care navigators as they’re embedded within an organization.
Significant Overall Savings
When members are referred to the right specialist the first time, it helps reduce duplicative care, eliminate care gaps, and ensure they get better faster. By getting them on the right track early in their care journey, the cost savings can grow quickly. In 2023, this food manufacturing company had over $1.2M in estimated annual savings achieved through optimized referrals.
1,532
Total Referrals Completed
1,064
Optimized Referrals
69%
Optimized
$1.2M+
Estimated Savings
Improved Member Care
Premise care navigators utilize our best-in-class data-driven referral matching and combine it with a hands-on, seamless concierge approach to provide members with the best experience possible. They handle everything from:
- Selecting a provider and facility
- Making the appointment
- Translating for the member as necessary
- Ensuring records are transferred before and after the specialist appointment
- Following up to support ongoing care needs
- Communicating with the member’s broader care team
With their onsite care navigator, the organization was able to provide this efficient care coordination and referral management for members within one to two business days, ensuring quick resolution when specialty care was needed.
The Importance of Efficient Coordination
The following member testimonial from this organization demonstrates the efficiency of care navigators when it matters most:
“A member came in for an annual physical on a Monday. Her lab studies showed iron deficiency due to abnormal blood loss during menstrual cycles. The provider consulted with the care navigator to request urgent referrals to gynecology and hematology. The care navigator was able to schedule the member with an OBGYN the next day, and hematology on Friday. This speed of service makes a critical difference in improving member care and ensuring positive outcomes.”
By expanding upon their existing primary care and pharmacy offering, this organization helped a large and diverse workforce properly navigate the US healthcare system and achieve their goals of improving member experience and reducing total medical spend. Through offering care navigation, a critical component of advanced primary care, members had access to a bilingual care navigator to lead a traditionally underserved population to the right specialty care.
In addition, the organization recognized significant savings through strategic navigation of specialty referrals. In helping many first-generation Americans get the care they need, the organization has firmly established its dedication to health equity and championing employee wellbeing through their partnership with Premise Health.



