How a financial services client saved $8.9M through the power of an advanced primary care approach
This Michigan-based financial services company has partnered with Premise Health since 2019 to offer better care for their people. In the years since, they’ve adopted the full advanced primary care model, which integrates multiple types of care into one coordinated experience. This approach has helped further reduce costs, create better health outcomes, and improve the care experience for their members.
The Challenge
With 29 million American adults unable to afford or access quality healthcare1, employers are feeling the financial impact of delayed health needs among their workforces. Estimates show that poor worker health costs organizations $575 billion a year, or 61 cents for every dollar spent on health benefits2. As healthcare costs and provider shortages continue to rise, organizations are searching for ways to improve care access in an increasingly challenging landscape.
One innovative financial services company wanted to proactively solve for their members’ gaps in care across various healthcare settings, which ultimately drive-up annual spend. With so many siloed point solutions in the market to juggle, this organization sought out a single integrated approach to make whole person care a reality.
The Solution
The partnership with Premise built towards an advanced primary care model, offering a holistic, coordinated approach across many types of care. This included:
>Primary care
>Virtual primary care
>Behavioral health
>Pharmacy
>Care management
>Care navigation
Additionally, complementary services like physical therapy were integrated into their offering. All of these types of care were made available to every employee for low-to-no out of pocket cost.
The Outcome
Through investing in whole person care, the organization saw massive savings attributed to the advanced primary care model. For the calendar year 2024, they achieved $8.9 million* in estimated savings, reflecting a 1.2x return on investment.
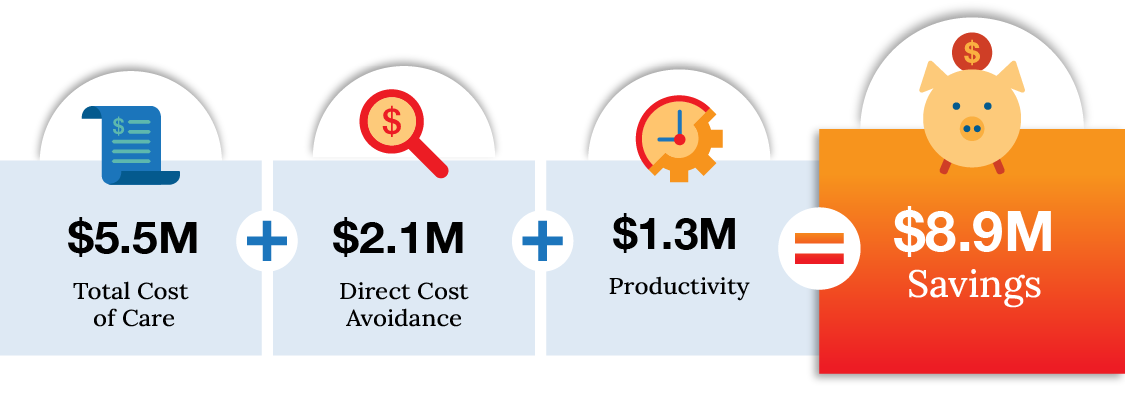
*Number reflects average savings and contains influence of physical therapy offering
Better value
More types of care =
more opportunity for savings.
When members engage with multiple types of care, they tend to be healthier and therefore less costly to cover over time. By offering a comprehensive and coordinated care solution to their population, the organization realized significant savings per member in 2024. For their 10,500+ eligible members, these savings increased as members engaged with more types of care in addition to primary care.
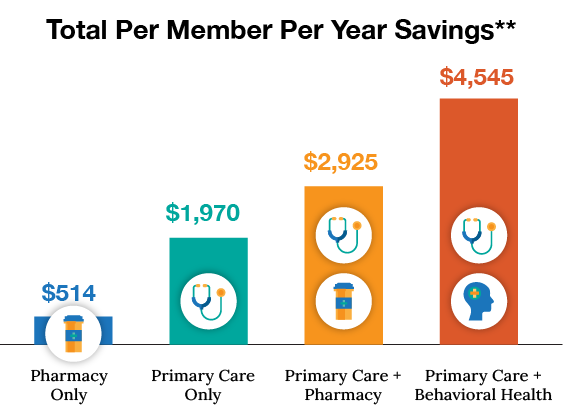
**Figures represent total cost of care savings, inclusive of all drug costs and medical expenses not related to clinic operation. It is not intended for comparison to any other marketing, feasibility or ROI calculations.
Better health
More preventive support =
less reactive care.
When great healthcare is just down the hall or a click away, members find it easier to make it part of their routine. Through more accessible primary care, Premise attributed members were using preventive services more, leading to healthier lifestyles and visiting the emergency room less. When members are able to address concerns early with a provider, they can get ahead of chronic conditions and avoid unexpected health events.
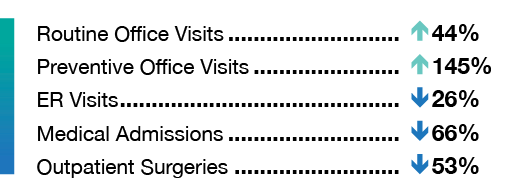
And utilizing preventive services more often means this client’s population was more up to date with their recommended screenings when compared to Cedar Gate national benchmarks:
more women’s health screenings among female population
more colorectal cancer screenings
The cost of preventable ER visits.

Avoidable ER diagnoses occur when a member receives emergency care for health issues that could’ve been treated with primary care.
In 2024, this organization spent $63,484 on avoidable ER diagnoses for Premise-attributed members compared to $186,108 for community-attributed members. This reflects a 63% lower spend achieved through just 26% fewer emergency room visits thanks to effective preventive care.
Improved chronic condition control.
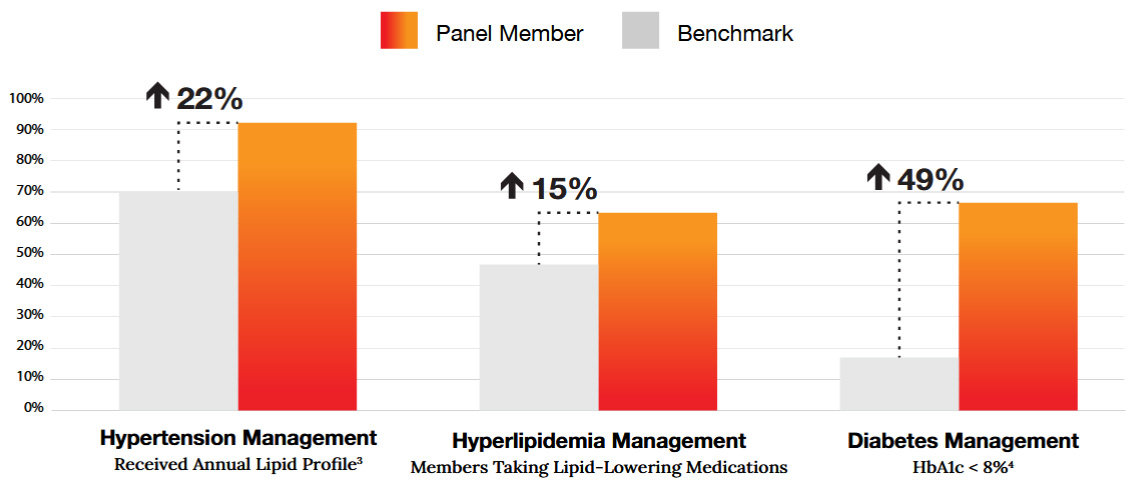
Care management offers personalized care plans for those with high-cost, high-risk conditions such as chronic conditions. Through the ongoing support offered by expert care managers, members managing chronic conditions gained better control of their conditions, seeing measurable improvements in critical health metrics:
More mental health support.
Care is most effective when it considers physical health as well as mental health and environment. Often the biggest hurdle to mental health support is finding a provider who can help. With behavioral health services readily available, members prioritized their mental wellbeing by scheduling and attending appointments and as a result saw a promising reduction in their depressive symptoms:
In Q4 2024, 95% of members with a completed depression screening had a recorded follow-up
appointment, up from 77% in Q4 2023
Premise-attributed members had 32% more mental health office visits than community-attributed members
With the support of behavioral health, 40% of members saw improvement in their depression questionnaire scores in 2024, reflecting a significant reduction in depressive symptoms


Improved member engagement.
When great benefits make member’s lives easier, word can spread quickly. This organization saw a large portion of their workforce take advantage of these benefits, with nearly all of their survey respondents reporting a positive experience and willingness to recommend the services:
In 2024, the organization had nearly a 30% penetration rate, meaning a third of members who were eligible to use the health center had at least one or more visits in the last 12 months
In 2024, 95% of members said they’d recommend this healthcare service to a friend or colleague
Enhanced access
Offering more flexible appointment options allows members to get care when they need it, wherever they need it. With virtual primary care, many members who may have otherwise delayed or opted out of care were able to speak with a virtual provider. Having both virtual and onsite options also opens availability for the rest of the member population, resulting in shorter overall wait times and a better experience for everyone:
Of all the primary care visits in 2024, over a third
were virtual (phone or video)
Wait time for primary care in 2024 was less than two minutes
Continuous care for specialist referrals.
For members needing referrals to specialty care, access to a concierge referral coordination solution helped guide them to high-value, or a combination of high-quality and low-cost, specialists and facilities. This ensures members have a seamless experience, as all administrative tasks like scheduling and follow-ups are managed by an expert care navigator:
Care navigators facilitated over 1,500 completed specialty care referrals in 2024
Additionally, a third of these referrals were made internally to a Premise affiliate, saving additional out-of-network cost and allowing for a more streamlined member experience
“I feel like the convenience and proximity to my job has been a big reason why I use the [wellness center] so much. Before, I would have to wait months or even longer to get into [my former provider] for a simple appointment. Even then I would have to leave work early to make it all the way out… for my appointment. The [wellness center] made it so easy to set up appointments and change them if needed…. [it] has been a game changer for my health!”
– Member in Michigan
By investing in advanced primary care for their population, this client saved millions in medical spend, saw their workforce get measurably healthier, and helped foster an exceptional member experience.
Through a whole person, coordinated care experience across multiple types of care, the advanced primary care model delivers on the promise of better value, better health outcomes, and better experiences.

1. Witters, D., & Maese, E. (2025, April 1). In U.S., inability to pay for care, medicine hits new high. Gallup.
2. Integrated Benefits Institute. (2021, March). The cost of poor health: Full cost estimator infographic [Infographic].
https://f.hubspotusercontent10.net/hubfs/8926463/IBI_March2021/New-Resources/Full-Cost-Estimator-Infographic-2020.pdf
3. Annual lipid profiles help identify and address lipid abnormalities as risk factors for hypertension
4. HbA1c of less than 8% in the last 12 months meets recommended HEDIS metrics on managing blood sugar level









